$15 treatment gets COVID patients off ventilators in under a week – study
if(window.location.pathname.indexOf(“656089”) != -1){document.getElementsByClassName(“divConnatix”)[0].style.display =”none”;}else if(window.location.pathname.indexOf(“/israel-news/”) != -1){ document.getElementsByClassName(“divConnatix”)[0].style.display =”none”; var script = document.createElement(‘script’); script.src = ‘https://player.anyclip.com/anyclip-widget/lre-widget/prod/v1/src/lre.js’; script.setAttribute(‘pubname’,’jpostcom’); script.setAttribute(‘widgetname’,’0011r00001lcD1i_12258′); document.getElementsByClassName(‘divAnyClip’)[0].appendChild(script);}
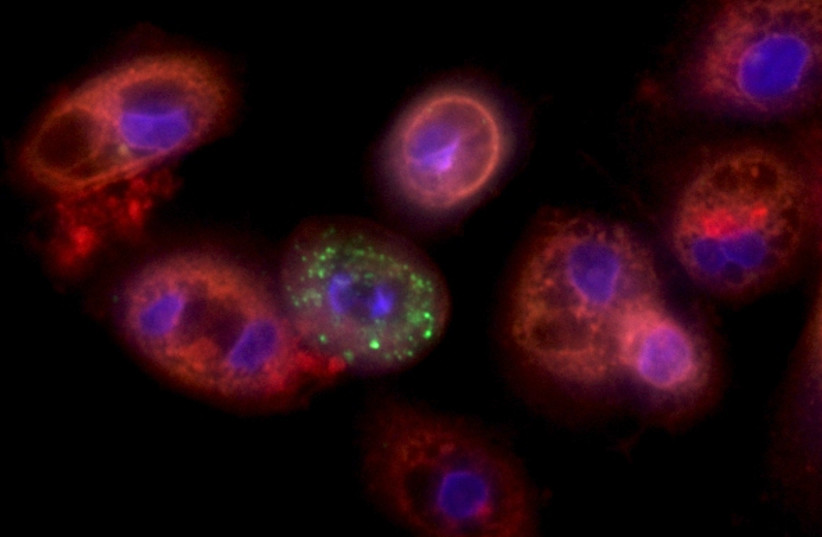 Lung cells infected with coronavirus (credit: YAAKOV NAHMIAS)
Lung cells infected with coronavirus (credit: YAAKOV NAHMIAS)




Comments are closed.