The War Doesn’t End. But as Long as He Keeps Fighting, I’ll Fight for Him, Too.
As of Jan. 17, veterans thinking about hurting themselves can get free crisis care, including inpatient, for up to 90 days at Veterans Affairs. They do not need to be enrolled in VA care. For immediate help, dial 988, then press 1.
My husband is thinking about hanging himself with the straps in the garage, so he asks me to hide them.
I tug the garage door upward, and its maw opens with a screeching yawn. The black nylon straps hang from a pullup bar. They bring back memories of CrossFit workouts with my husband, and our post-workout smiles as we dropped to the floor exhausted but victorious.
Now these straps represent potential suicide. My best friend—a war veteran, and the person I love most—doesn’t want to live anymore. I need to pull myself together, and I’m barely hanging on.
I take a deep breath, tell myself not to panic. He needs me, and I can get through this because now I know how to get help. For so many years, I didn’t know.
The black nylon straps and rings in the Flores family garage brought back memories of CrossFit workouts. Then Sarah Flores’ husband told her he was thinking about using them to hang himself. Rings by Sarah Flores.
I hide the straps in a forlorn plastic tub, in a stuffed corner where the dust and black widows keep it company. Then I join my deflated husband at our dining table. His exasperated breaths are like a series of exhales, without the inhales to fill him back up. As I listen to him speak, I feel his emptiness, how he clings to life.
It is August 2019, more than a decade since he returned from war, a decade of wayward paths that dabbled in wedding photography, volunteering as a reporter at a local radio station, and years languishing at the house as a stay-at-home dad. In a month, he’ll return to the university for a third time to finish his bachelor’s degree.
Despite years of devastating failures and academic probations, he kept turning back to his sociology degree, dreaming of becoming a professor and teaching the Iraq War. We have learned how to manage his anxiety and depression, and I am confident that this time he will find success. We are so close, only one month from what I know will give him joy and fulfillment. I believe in him. I always have.
But I can’t make him believe in himself. Hunched over the table, he speaks of regrets, failures, and thoughts of suicide. This is actually a good thing, that he can talk to me. He used to keep these thoughts secret.
I met Mike in a college dorm. My roommate and I had finally built up the courage to open our door. He was the first to poke his head into my room, flashing a cheesy grin. “Hi, I’m Mike!”
The nerve.
Over the next few months, Mike continued to poke his head into my room. He loved to interrupt my studying, be my gym coach, and nudge this introvert to Halloween parties. We often took late-night strolls around our college campus, discussing our love for Star Trek, why I was majoring in computer science, or why he enlisted in the Army National Guard—a part-time obligation—at the age of 17. I was fascinated. I had never known anyone in the military.
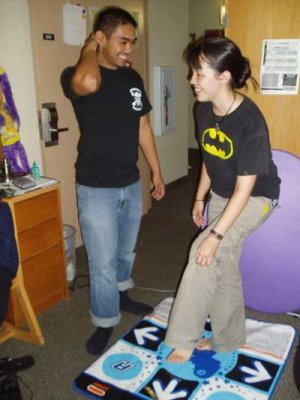
Sarah and Mike Flores play Dance Dance Revolution in their college dorm room, where they met. Mike was in the Army National Guard, and he deployed to Iraq as a combat medic a year after they met. Photo courtesy of the author.
A year after we met, Mike stopped visiting my room. He had deployed to Iraq as a combat medic. We exchanged letters, chatted for hours on instant messenger, and I kept my phone glued to my side. I wondered if he also noticed Orion in the sky, only half a world away.
I yearned to hear his laughs, those full-body barks of joy that were on the edge of obnoxiousness. How he danced like no one was looking, even when everyone was. How he would halt abruptly in a crowd to patch up an old lady who slipped on the steps or drive an hour in traffic to fix his mom’s printer.
Now he was at Camp Bucca in Iraq. Sometimes weeks passed without contact, with only teasing gut punches of seeing his doppelgangers in the park—complete with khaki shorts and striped polos. He did return, after a grueling 12 months.
But now he was often tense, quick to anger, and dropped to the floor at the sound of a firework. He was haunted by the soldier he couldn’t save.
During his deployment, I had grown more independent, blossoming into a young adult who now had the courage to move away for a summer internship. I was concerned about how Mike had changed, but I had also changed. When we talked about marriage, I told him he would have to choose the Army or me. I didn’t want to be a military wife, and one combat deployment was enough. We got married later that year.
At the time, I didn’t think too hard about our wedding vows, how we promised to stay together “in sickness and in health.” I thought it meant physical health, not mental or emotional. I had no idea the war would torment us, testing our marriage.
It began in our first years—it became our trial. The secrets and lies; unnecessary purchases that we now recognize as manic spending; years of lying in bed and playing video games instead of going to his university classes; the agonized screams as I cradled him close through the nightmares.

Sarah and Mike Flores before Mike left for Iraq. Photo courtesy of the author.
I thought we were managing until our first daughter was born. That was when everything ignited. Our newborn pushed us to our limits as new parents. We didn’t know how best to soothe her frequent crying, or how best to position a sleepy baby in a crib that might suffocate her. The days blurred together—days and nights intertwining—in a haze of tense exchanges, helpless sighs, and grated nerves.
And Mike was a powder keg—not the man I married, his body stiff, his frustration palpable, his red eyes aflame with anger that shook me to my core. I had never seen him like this. The rage contorted his face as he tightened his grip around our sobbing daughter, willing the cacophonous screams to stop. I snatched the baby back, pointing him to the other room and telling him to close the door behind him. It didn’t matter how exhausted I was; I did what I had to to keep our baby safe.
Eventually, Mike became scared of himself. His love for our daughter pushed him to finally get help. With the aid of the VA’s therapists and psychiatrists, we discovered that Mike had post-traumatic stress disorder, depression, anxiety, bipolar disorder, and more. The VA assigned him a “permanent and total” disability rating, like it’s not going away, and he’ll live with all of this for the rest of his life. The war doesn’t end.
He committed to treatment, and I did it all. I supported our family with a full-time job, raised our kids, and ran our household. I also frequently cried in the car, or in the shower, or in a bathroom stall at work. For years, I felt alone and terrified. No one around me understood, especially our families who lived an hour away. They told us to pray, or they blamed my husband as if he asked for this.
Award-Winning Journalism in Your Inbox
I once thought about leaving, but as long as Mike kept fighting for himself, I would fight for him too. Our bond grew stronger. I spent the following years walking on eggshells around my husband, learning how best to manage his conditions with him, and handling most of the child care. This was survival mode, and this overachieving, straight-A student wouldn’t be defeated.
After nine years of marriage, a VA nurse sat at our dining table and asked Mike to leave the room. She asked me questions about my stress levels as a caregiver. It felt strange to have someone focus on me instead of my husband. As I answered, her pencil flicked off checkboxes on the paper in front of her. Then she paused.
She exhaled, set down the pencil, and met my gaze. “You are heavily burdened,” she muttered as she took my hand. Her voice was soft and her eyebrows furrowed with compassion. “I’m so sorry.”
I opened my mouth to speak but didn’t know what to say. As her words began to register, I trembled, trying to breathe through the sobs. This woman understood all my years of pain and struggle. This was the validation I didn’t know I needed.
She explained that I could get help through the VA Caregiver Support Program and connected me to resources. I signed up for everything at once: individual therapy sessions, an online caregiver workshop, and a caregiver support group.
Within weeks, I sat at a conference table, shifting in my seat and exchanging furtive glances with strangers. I had never been to a support group before. Nearly all of them were caregivers for elderly parents. After the session, the social worker pulled me aside.
“You are on the path to depletion,” she said with piercing eyes and a graveness that made me pause. I didn’t want to believe her. I thought I was doing all right. I was working my dream job as a software engineer at NASA, sleeping well, exercising, eating healthy, spending quality time with my kids, and street painting multiple times a year at chalk festivals. I told myself I was just doing the super mom thing. I was in denial.
The social worker’s words sank in that evening. The weight of six years of caregiving dragged me into dark depths. I’d never fallen this deep, drowning under the crushing weight of all the work, burdens, my endless responsibilities. Mike sent the kids to our parents, and I cried in bed for hours. I was so tired of being strong.

After more than a decade of mental health struggles related to his time as a combat medic in Iraq, Mike Flores finished his master’s degree. “I couldn’t do this without my wife,” he said. Photo courtesy of the author.
My body felt heavier and hard to move, my willpower drained. I wondered if this was what depression felt like. My husband held me tenderly and sighed, “I know how you feel.” That made me cry even more.
He searched my face with wide eyes. “Did I do something wrong?”
“No, you didn’t,” I laughed through my tears, “and I know exactly how you feel.” For one bittersweet moment, our roles were reversed—he was the caregiver now. We had a newfound appreciation for the other’s struggles. I just wanted to feel cared for too. We focused on giving me more breaks, and I learned to build my village of support, people I could call on for help in times of need.
Now, a year later, I need that village. After hiding the straps in our garage, I leave my suicidal husband at the dining table, move to the living room to cry for a bit, then call his therapist. No answer.
I try the VA caregiver crisis line, and they recommend I take him to the psych ward. Like a mental hospital? I picture a gothic asylum with patients in white straitjackets, crazed zombies stumbling down fluorescent halls. Do I really drive Mike to a mental prison? This feels wrong.
I collapse at home, knowing I must process my feelings and ask for help. The next few days are a blur: a tearful huddle with close friends at midnight, while we savored the crispy Asian chicken and boba drinks they brought me. A heartfelt talk and embrace with my next-door neighbor, before he walked my dog. My nervous breakdown at the gym, amongst my group of mom friends.
“What happened?!” they pleaded with distressed faces. One of them brought me a homemade dinner the next day.

Sarah and Mike Flores today. Photo courtesy of the author.
I tried to stay calm as I explained to my family. To our six- and four-year-old daughters, “Daddy is very tired. He needs to go to the doctor for a while so that they can help him find energy again.” To my stoic but supportive parents: “Thank you so much for watching the girls. I’m going to be OK.”
I pick up Mike from the psych ward about a week after he’s admitted. The next month, he makes it back to school. Then two years later, he finishes his degree, which took over 15 years of struggle.
It’s a beautiful day in our grassy backyard, surrounded by our village of family and closest friends. Mike makes a speech in front of the crowd—it’s his graduation party, after all. “I couldn’t do this without my wife,” he gestures at me, sitting in the audience. My friends hold me while I cry happy tears.
Our Journalism Depends on Your Support
I’m proud of how far we’ve come. Our challenges won’t end, but I know everything will be OK because we have each other. Mike and I are a team, and we’ve become an amazing one.
It just took a big dose of healthy communication and two stubborn people to overcome their denial to get there.





Comments are closed.